FAI - Femoroacetabular Impingement
What is It?
- FAI is a recently understood hip condition which describes a mechanical mismatch between the ‘ball’ and the ‘socket’ of the hip
- There are two described types of impingement:
- ‘Cam’ type impingement describes a ‘bump’ on the surface of the femoral head (ball) which jams on the rim of the (acetabulum) socket
This typically affects younger athletic men (common)
- ‘Pincer’ type which described an overdeep acetabulum (socket) which restricts the movement of the femoral head (ball)
This typically affects middle aged women (less common)
- ‘Cam’ type impingement describes a ‘bump’ on the surface of the femoral head (ball) which jams on the rim of the (acetabulum) socket
- Often there is a degree of overlap between the types
Normal Hip
- Normal hip showing the femoral head and neck (ball), acetabulum (socket), and the labrum (fibrous rim of the socket).
- Normal range of flexion and rotation is achieved without impingement
 |
 |
 |
No impingement with flexion, adduction and internal rotation |
Cam Impingement
- Hip showing the femoral head and neck (ball) with impingement lesion (bump), acetabulum (socket), and the labrum (fibrous rim of the socket).
- Limited range of flexion and rotation is achieved without impingement – causing pain and reduced hip flexibility
 |
 |
 |
Impingement of the femoral neck ‘cam’ with the acetabulum with flexion adduction and internal rotation |
Pincer Impingement
- Protrusio hip (deep socket) showing the femoral head and neck (ball), deep acetabulum (socket), and the labrum (fibrous rim of the socket).
- Very limited range of flexion and rotation is achieved without impingement – pain and stiff hip
 |
 |
 |
Impingement of the femoral neck on the ‘pincer’ of the acetabular rim with flexion adduction and internal rotation |
What are the Symptoms
- FAI often presents as hip and groin pain with restricted range of hip movements.
- Symptom onset can be acute, following injury, or insidious after prolonged exertion. It is generally not disabling, except in sporting activity.
- ‘Payback pain’ after participating in sporting activity is common
- Pain is primarily felt deep in the groin at the front of the hip, more rarely it can be on the side of the hip or the buttock.
- Movements can be restricted particularly high flexing and trying to cross the legs.
- Pain is often provoked by these manoeuvres, by exercise, or by attempted return to sport and relieved by rest and inactivity.
- FAI may occasionally present as groin pain after prolonged sitting. There is no rest or night pain.
What Else Could it Be?
- Groin pain has many causes, only through a thorough history and examination, often with further investigations can the underlying cause be diagnosed.
- Alternative diagnosis includes:
- Muscular, tendinous, ligamentous and bursal inflammation around the hip, including bruises, strains, and sprains.
- Bony injuries can include physeal and apophyseal injuries in children, and fractures, subluxations, and stress injuries,
- Infection and inflammatory conditions in adults.
- Intra-articular pathology such as avascular necrosis, labral tears, loose bodies and infection must also be excluded.
- Finally pain may be referred from the lumbar spine, ilioinguinal and lateral femoral cutaneous nerves
- Muscular, tendinous, ligamentous and bursal inflammation around the hip, including bruises, strains, and sprains.
Examination Findings
- Patients characteristically point to the source of pain with two fingers or cup the trochanter with the thumb and index finger ‘the trochanteric ‘C’ sign’.
- Diagnosis is 90% positive with reproduction of their symptoms on the Impingement test – flexion adduction and internal rotation of the hip.
- Provocation of pain by flexion abduction and external rotation i.e. sitting cross-legged may provoke pain but is generally non-specific.
- There may be some restriction of movement at the extremes of hip internal rotation and flexion.
Why?
- It is clearly understandable when looking at the schematics how impingement occurs, the unknown question is why?
- It is believed that many normal people have ‘bumps’ or slightly over-deep sockets and could potentially develop FAI – this is just the way we are built and develop.
- But the hip has to also be provoked in some way to cause damage – this explains the tendency for athletes, sporting professionals and active people to be more susceptible to this form of injury.
Signs of Pain
- Anterior groin pain, and the trochanteric ‘C’ sign
 |
|
 |
|
Tests and Investigations
- AP x-rays of the pelvis and lateral x-rays of the hips are the first line of investigation
- The femoral head may show the characteristic pistol grip deformity, a flattened head/neck junction, loss of sphericity or herniation pits.
- The acetabulum may show specific abnormalities such as the os acetabulare, ossification of the acetabular rim or the cross-over sign of posterior and anterior acetabular walls.
- A standard hip MRI scan, magnetic resonance arthrography and high resolution 3-D CT scanning are the specialist investigation of choice usually under the direction of an orthopaedic surgeon in consort with a radiologist with an interest in young hip pathology.
 |
 |
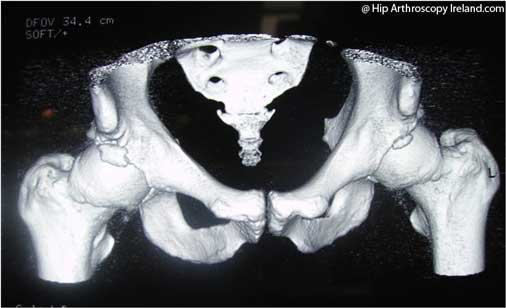
3-D CT Scans of FAI
- 3-D CT scans of the pelvis showing ‘cam’ and ‘pincer’ impingment lesions, and os acetabulare
 |
 |
MRI Scan of FAI
- MRI of the hip showing ‘cam’ impingement lesion and associated labral pathology
 |
 |
MRI Arthrogram of FAI
- MR arthrograms of the hip showing labral tears and FAI
 |
 |
Management
- An initial trial of non-operative treatment is advocated for most patients as the pain is relatively self-limiting.
- Lifestyle modification is the single most important factor. For most this may result in resolution of symptoms but this will restrict attempts to return to sport.
- Use of painkillers and anti-inflammatories may temporarily help the pain
- Physiotherapy may reduce the local inflammatory reaction, improve core stability, improve soft tissue flexibility and assist in measures to avoid provocation but will not address the underlying mechanical problem.
- Labral tears, like meniscal tears can heal with time, but the underlying anatomical lesion (i.e. impingement) remains unchanged and return to sport usually provokes symptoms. Treatment of this lesion requires surgery.
Surgery
- Referral to an orthopaedic surgeon with an interest in young adult hip pathology is the pathway toward successful resolution of symptoms
- Surgical treatment is performed either by arthroscopic debridement or can be performed by open surgical debridement.
- While the techniques are quite different, the operations both aim to address the mechanical and pathological changes around the neck/acetabulum junction.
- Hip arthroscopy techniques permit examination of the femoral head, neck and acetabulum through a series of portals ‘keyholes’. The technique can treat labral tears, loose bodies, ligamentum teres lesions, cartilage flaps and impingement lesions and much more. It is possible to excise the impingement bump and excise the ‘pincer’ by acetabular rim recession.
- The surgery is usually carried out as a day case, recovery usually takes three months.
- Open hip debridement, an extensive open procedure for FAI which similarly exposes the complete hip joint, where, under direct vision, while protecting the vulnerable femoral head blood supply, the impingement lesion and ‘pincer’ are excised, recovery usually takes 12 months
- A further open procedure which is not possible by arthroscopy is re-orientation of the acetabulum by periacetabular osteotomy. With open surgery post-operative recovery can exceed 18-months.
- Surgical treatment is not undertaken lightly and should only be performed by orthopaedic surgeons with a subspecialist interest in young hip pathology with experience of open and arthroscopic techniques as there is a steep learning curve and risk of significant complications.
Arthroscopic surgery for FAI
- FAI at arthroscopy showing labral tear and ‘cam’ impingement lesion
 |
 |
Results
- Arthroscopic treatment is the preferred surgery performed by the author
- Excellent results can be achieved with arthroscopic treatment of FAI; recovery steadily improves post-operatively, 80% of patients are cured by 3-4 months and with up to 95% having improved symptoms by one year
- 5% of patients have a complication related to surgery
- This compares very favourably with open surgery (either debridement or peri-acetabular osteotomy)
Rehabilitation
- Rehabilitation is an essential part of the recovery following surgery for FAI
- Recovery from hip arthroscopy is typically 3-4 months
- Recovery from open hip debridement is typically 12 months
- Recovery from peri-acetabular osteotomy is typically 18 months
- A working knowledge of FAI and familiarity with the rehabilitation program following surgery is a great advantage for the physiotherapist
Hip arthroscopy rehabilitation
- I use a program developed by Mr R Villar and Pure Sports Medicine in London (reproduced with permission)
- Essentially there are two pathways of physiotherapy, ‘Fast track’ and ‘Slow track’
- ‘Fast track’ is for patients with FAI who have a limited amount of surgery in their hip for example, labral debridement, moderate impingement lesion excision, and modest chondroplasty. They spend four days toe-touch weightbearing on crutches
- ‘Slow track’ is for patients with FAI with greater amounts of surgery or when natural healing processes need a chance to complete before accelerating recovery for example, labral repair, subchondral microfracture, acetabular rim recession, large impingement lesion excision, or other soft tissue procedures in the hip. They spend four weeks on crutches toe-touch weightbearing.
‘Fast track’ physiotherapy program
Slow track physiotherapy program
Case report 1- Patient with FAI
- Mr B is a 30-year-old male who played county gaelic football and is a part-time mechanic. He trains or plays at least four times per week. He complains of a six-month history of right groin pain, of insidious onset, precipitated by running and twisting at speed in training and high flexing when kicking and often lasting for 12-24 hours after a vigorous match or training session. The pain is occasionally associated with clicking within his hip. The pain is localised deep inside his hip and he grips his trochanter as he tries to describe its location. Usually pain is temporarily relieved by simple analgesics, and rest. He has attended the club physiotherapist for two courses of physiotherapy and completely abstained from all sport for six weeks and found the pain disappeared but on return to his training symptoms return as before.
- There is no previous history of trauma, nor of pre-existing hip problems. He is fit and healthy, with virtually no contact with the medical services. He is concerned that he may have ‘early arthritis in his hip.’ On examination he has no hernias, no mechanical back pain or other external causes of groin pain. His hips move through a pain-free arc in extension but you note on the right there is limitation and irritability of the hip in full flexion, adduction and internal rotation. This reproduces the pain he reports. Plain AP and lateral radiographs of his pelvis are reported as normal. MRI scanning reveals a labral tear and anterosuperior impingement lesion on the femoral neck.
- Referral to an Orthopaedic surgeon with a subspecialist interest in hip arthroscopy is recommended
Case report 2 – Patient with FAI
- Miss H is an active 34-year-old solicitor who plays first XI level hockey and runs half marathons. She presents with three months of right anterior hip pain. The pain lies deep in the groin and she localises it by cupping her hand over the greater trochanter. Pain is precipitated by bending to hit the hockey ball or running any distance. Often it is after a game when she is most limited. She has had to miss the end of the hockey season and give up her plans to run a local marathon. Her physiotherapist has used a variety of techniques including manipulation and stretches which fail to resolve the pain. She takes simple anti-inflammatory medication to ease the pain. More recently she has found the 20-minute walk to work a struggle.
- She has no significant past medical history, no previous injuries though she mentions a period during her university years when the ‘hip hurt for a while’. Her clinical examination is again characterised by a positive ‘impingement sign’ where in high flexion, adduction and internal rotation the hip pain is exactly reproduced.
- An x-ray of her pelvis is reported as showing mild acetabular dysplasia but no significant abnormality. An MRI scan shows a labral tear, a paralabral cyst and early chondral damage in the anterosuperior acetabulum.
- Referral to an orthopaedic surgeon with a subspecialist interest in hip arthroscopy is recommended.




